Survey results: Indigenous Cultural Safety, Cultural Humility, & Anti-Racism Standard of Practice
On September 30, 2022, 11 BC health profession regulatory colleges adopted an Indigenous Cultural Safety, Cultural Humility, & Anti-Racism Standard of Practice (PDF). The standard sets clear expectations for how registrants are to provide culturally safe and anti-racist care for Indigenous clients and patients. In February 2023, 10 colleges – including CDOBC – circulated a survey on the standard to their registrants.
With input obtained through the survey from both Indigenous and non-Indigenous registrants, we are better able to interpret information that has been self-reported and understand the areas in the implementation of the standard where clear focus is required. We thank all survey participants and provide a summary of what we learned.
National Indigenous Peoples Day
June 21 is National Indigenous Peoples Day. CDOBC is honouring the day by affirming the College’s commitment to support Indigenous cultural safety, cultural humility, and anti-racism in BC’s health care system through initiatives including the Standard of Practice and survey.
Survey goals
Through the survey, the colleges aimed to establish a baseline of non-Indigenous registrants’ attitudes, perceptions, and perspectives related to Indigenous-specific racism in general and particularly in healthcare settings. The survey will be re-administered to measure change over time.
The colleges also aimed to gather information from Indigenous and non-Indigenous registrants about barriers to the implementation of the standard in their practices, and their learning needs related to the standard’s core concepts.
Respondents
A total of 3,361 registrants from the ten colleges, representing 12.2% of those who received a link to the survey, responded to the survey. Three percent (3%) of respondents self-identified as Indigenous.
Survey development
The survey questions were developed collaboratively by Pivotal Research Inc., Qoqoq Consulting Ltd. (Indigenous consultant Joe Gallagher), and the 10 participating colleges. Included were questions about:
- Attitudes and perceptions about Indigenous-specific racism
- Perspectives on Indigenous-specific racism in healthcare settings
- Current behaviours that reflect each principle of each core concept of the practice standard
- Implementation of the practice standard
- Guidance and/or education required to implement the standard
- Learning intention (when learning will begin)
- Preferred education delivery method
- Overall perceptions about the new standard
- Behaviours observed in practice settings (Indigenous respondents only)
- Stereotypes of Indigenous peoples (non-Indigenous respondents only)
Non-Indigenous respondents were asked to consider their own attitudes, perceptions, perspectives, and behaviours; Indigenous respondents were asked to consider the attitudes, perceptions, perspectives, and behaviours of non-Indigenous colleagues in the same profession. Some questions were asked only of non-Indigenous respondents; others were asked only of Indigenous respondents. A trigger warning was included in the introduction of the survey, recognizing that some statements could be harmful.
Trigger warning: The results described below contain statements and descriptions of racism and negative experiences that may be triggering to some.
What we learned
The following results summarize the themes within the responses. While there were some differences in responses between colleges, these were not substantial enough to warrant reporting separately. In general, input was similar regardless of health profession.
- There is a continuum of attitudes and perceptions about Indigenous-specific racism reported by non-Indigenous respondents. Some agreed or strongly agreed with statements that represent stereotyping and contribute to perpetuating unsafe care and health inequities for Indigenous people. For example:
- 7% of non-Indigenous respondents strongly agreed/agreed with the statement “Colonialism is old news, we’ve all lived here for hundreds of years now, Indigenous Peoples should get over it.”
- 10% of non-Indigenous respondents strongly agreed/agreed with the statement “As a society, we’re being too accommodating to Indigenous Peoples.”
- 20% of non-Indigenous respondents strongly agreed/agreed with the statement “Indigenous people have problems with drugs and alcohol.”
- 13% of non-Indigenous respondents strongly agreed/agreed with the statement “Indigenous people get a lot of stuff for free that others have to work hard for.”
- The longer a non-Indigenous health professional has been in practice, the more likely they are to:
- say leaders in the workplace setting have set accountability outcomes to ensure the elimination of Indigenous-specific racism.
- agree with the stereotype that Indigenous people have issues with drugs and alcohol.
- indicate they learn about Indigenous communities located where they work.
And the less likely they are to:
- report acts of racism to leadership and/or the relevant health regulatory college.
- believe the new standard should have been adopted much sooner.
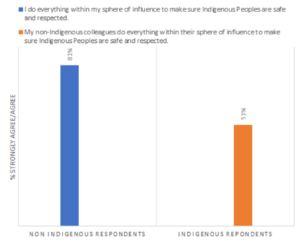
- The attitudes, perceptions, perspectives and behaviours of non-Indigenous respondents as self-reported differ from the words and behaviours observed by their Indigenous colleagues. This was consistent to various degrees throughout the results. While many non-Indigenous respondents believe their intentions and actions reflect safe and respectful care, the impact of their actions, as noted by Indigenous colleagues, is often not what it is believed to be. For example:
- Indigenous-specific racism exists beyond public healthcare settings. Eighty percent (80%) of all respondents recognize that Indigenous-specific racism is a problem in public and private healthcare settings alike.
- Commonly reported barriers to implementation of the new standard were competing priorities, overwhelming workload, and being unsure of what learning opportunities are available/appropriate. However, 33% of respondents reported they have no barriers to implementation.
- Between 13% and 31% (varied by core concept) of respondents require further guidance and education to implement the standard. The preferred delivery methods for educational offerings were webinars and short reads. Of those who indicated a need for further guidance and education, 50% intended to start or continue their learning within three months.
Summary
These results provide an important baseline measure of attitudes, perceptions, perspectives, and behaviours of health profession registrants against which progress and change will be measured in the future.
The value of participation by self-identified Indigenous respondents cannot be overstated. As health professionals and health profession regulators work to ensure Indigenous clients and patients receive culturally safe care, only Indigenous clients and patients can confirm we have achieved that outcome. Indigenous health professionals help the colleges understand and reflect upon our progress, or lack thereof, by offering their perspectives on how their colleagues and the system are performing.
Next steps
The results also provide insight to health profession regulators about the barriers to implementation of the standard and the guidance and education that our registrants need to move forward with implementation. We will work together to meet those needs.
Standard of Practice and learning resources
Registrants are encouraged to become familiar with the content, expectations, and intent of the Indigenous Cultural Safety, Humility, & Anti-Racism Standard of Practice (PDF) in order to meet regulatory commitments.
Additionally, the BC College of Nurses & Midwives and the College of Physicians and Surgeons of BC have provided access to resources they created to support registrants with the Indigenous Cultural Safety, Cultural Humility and Anti-racism practice standards the colleges introduced in February 2022:
Videos:
- Introduction to the standard
- Self-reflective Practice(It starts with me)
- Building Knowledge Through Education
- Anti-Racist Practice(Taking action)
- Creating Safe Healthcare Experiences
- Person-Led Care(Relational care)
- Strengths-based and Trauma-informed Practice(Looking beneath the surface)
